Keeping patients comfortable with conventional dentures that rest on less-than-ideal ridges is becoming increasingly more difficult. Severe atrophic ridges and thin mucous membrane areas are a daily challenge for denturists because patients expect comfort from their dentures, despite their compromised oral condition. Although dental implants are the optimum treatment option, many patients choose not to have implants placed for a number of reasons. In such cases, an alternative must be found to assist the patient. Although soft lining material is in no way a substitute for dental implants, it is an attempt to keep the patient as comfortable as possible. Soft liners have had a long-standing role in the dental profession in varying applications. I have used a variety of soft liners over the decades and have had challenges and limitations in their use. I gave up in frustration, shying away from using them as a temporary or long-term laboratory technique because ultimately they posed problems, despite the promises made by the manufacturers. In 2003, a colleague gave me a package of soft lining material to try. I was very skeptical. In fact, the material sat on my shelf for nearly eight months before I used it. One day in desperation, I used the material on a full lower denture in a laboratory technique. I was impressed by the bonding strength to the denture base and how easy it was to use. I started using the material on selected patients over the next few weeks to ensure the material was as effective and lived up to the manufacturer’s promises. The patients were recalled every few months for two years to ensure that the soft lining material did not harden, de-bond or crack as many other materials have done. I evaluated the material and the comfort of the patient. I was so impressed by the material that I decided to use this product on all my patients who required a soft liner. The manufacturer recommends it as a chair-side material as well, so I began using it on immediate cases as a temporary liner – both for extractions and implant placement. Although this article is primarily about the possibilities of EasySoft liner™, it may also, be beneficial as general information about other soft lining materials. Categorizing the materials helps clinicians to understand how the soft lining material will perform for the task it is chosen for. This alone can save valuable chair time and decrease frustration for both the denturist and patient. The categories are 1. chemical composition, 2. chair-side versus laboratory use, 3. temporary versus permanent (long-term use). There are basically three different chemical compositions in soft lining materials used today. The first chemical composition: plasticizers are a liquid and powder formulation. Some of these plasticizers can be used both in chair-side and laboratory procedures. For chair-side procedures, these soft liners are often chosen to secure immediate dentures during the healing process or in an implant overdenture prosthesis during osseointegration. These materials are used widely throughout the dental industry as a quick-fit-fix in a chair-side procedure. Plasticizers are also used as tissue conditioners in preparation of the oral mucosa prior to taking final impressions. A disadvantage to these materials is that the liquid (ethyl alcohol) leaches out of the lining into the patient’s mouth and is then replaced by saliva and bacteria.
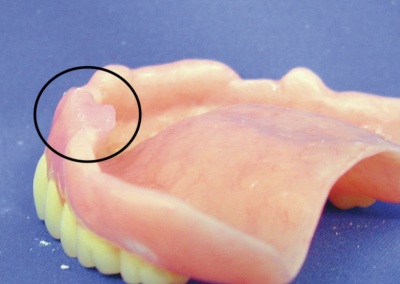
Fig.1 Problems of placticizer soft liners – material will harden, crack, and cause oral hygiene concerns and irritated tissue.
Problems of placticizer soft liners – material will harden, crack, and cause oral hygiene concerns and irritated tissue.
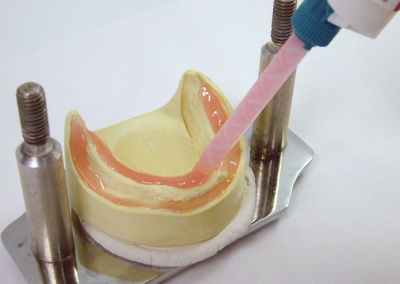
This causes the soft lining to become brittle and rough, leading to sore spots and tissue irritation. (See Fig.1 on the previous page.) Chair-side plasticizers quickly lose their soft properties and ideally should be changed every two to three days. Most of these plasticizers do not require an adhesive, therefore a strong chemical bond to the acrylic base is not achieved and the liner often peels away within a short period of time. Some of these soft lining materials use dibutyl phthalate as a plasticizer. Dibutyl phthalate is also used in many non-dental products as a softener (plasticizer). These non-dental products include some nail polishes and hair sprays. Dibutyl phthalate is a known carcinogen. The second chemical composition: HTV (Heat Treated Vulcanite) Molloplast®B is the best known HTV. This one paste formula requires high heat to cure and adhere to the acrylic denture base. Due to the high heat needed, it can only be used in a laboratory procedure. Some denturists/technicians find some challenges with this kind of material, as the bonding to the denture base material can be technique sensitive. An adhesive is recommended with this material and when used with success is effective. Other users prefer to use new denture base material to form a chemical bond. Sometimes during the trimming and pumicing stage, if too much heat is generated, the material may peel away from the denture base. The third chemical composition: the new generation of soft liners, such as EasySoft liner™, are silicones (A-silicone), also known as VinyPolylSiloxane or VPS. These new materials are dispensed in a cartridge system similar to silicone final impression materials. Due to the versatility of some of these silicones, they can often be used in both chairside and laboratory procedures. Because of these qualities, silicones are fast replacing the previously used materials that have dominated the industry for decades. They are often referred to as the “second generation of soft liners.” Once you have determined what chemical composition you would like to use, you may classify the material further into two other categories: chair-side procedure versus laboratory technique. Chair-side is also referred to as direct procedure, as you are working directly on the patient to perform this procedure. The proper handling of material and desired thickness is often compromised working directly on the patient because bonding is sometimes affected due to saliva. Some clinicians have had good success with chair-side soft liners, while others find it challenging. For temporary soft lining, it is obvious that chair-side use is the
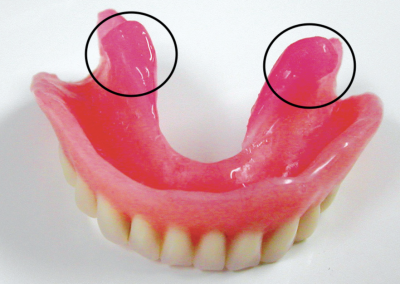
Fig.4 Undercuts are utilized for retention, supported lingually by acrylic and remain comfortable and won’t de-bond.
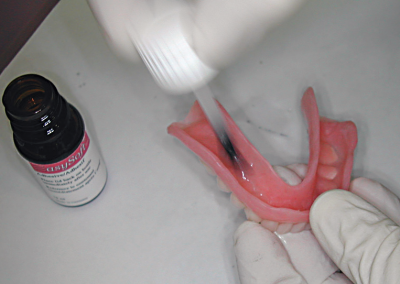
procedure to use, recurring the patient at a later date to permanently reline or rebase the denture. The laboratory technique is certainly the recommended way to do permanent (long-term) soft liners. The laboratory setting allows the denturist/technician to handle the material in an optimum manner to control the thickness of both base material and soft liner and to increase the bonding strength between the two materials. Some adhesives or bonding agents adhere better and longer if a higher temperature other than the patient’s body temperature is utilized. The final classification to further determine your material choice is temporary versus permanent soft liner. Although there is no question of what the word temporary means, the word permanent has a misunderstood meaning in the industry. Permanent does not mean the material will be permanently attached to the denture base material nor will the material last forever. Manufacturers use the word permanent to describe the material remaining permanently soft. Perhaps we should consider using long-term soft lining instead of permanent when determining the length of time the soft liner is desired.